With climate change recognised as one of the greatest threats to human health, dietitians are increasingly being called upon to play a role in helping the NHS and wider food system reach Net Zero targets. But how well equipped are dietitians to meet this challenge, what actions are they already taking, and what barriers stand in the way? This blog shares insights from an undergraduate dissertation that set out to explore these questions, offering a snapshot of knowledge, practice, and opportunities for the future.
By Anna Catling, BSc Hons Nutrition and Dietetics

Why Climate Change Matters for Dietitians
Climate change is an urgent threat to both human and planetary health.7 Limiting global warming to 1.5°C above pre-industrial levels could reduce the risk of irreversible impacts, yet by 2024, global temperatures had already risen to 1.6°C.1
Climate change is already adversely affecting human health, and these impacts are expected to worsen, for example, through increased rates of heat-related or respiratory illness and non-communicable diseases.19 These climate-sensitive health risks will contribute to growing pressures on the NHS (National Health Service) and could exacerbate barriers to healthcare.12,19
The UK food system is responsible for 19% of the nation’s greenhouse gas emissions, rising to nearly 30% when imports are included. Healthcare contributes a further 4–5% of emissions.1,9 Working in food and healthcare, dietitians are in a unique position to cut carbon and improve health. The Health and Care Act 2022 makes it a legal requirement for the NHS to act on climate change, with targets to cut emissions to Net Zero by 2040 for those it controls directly, and by 2045 for those it can influence.7,12 This raises important questions: What actions are dietitians currently taking to contribute towards Net Zero? What barriers are limiting progress? And how is the profession evolving to meet the demands of a low-carbon future?
To find out, I distributed a questionnaire to registered dietitians via the BDA website, LinkedIn, and personal contacts. It explored topics such as Net Zero–related knowledge, perceived importance, education and training, views on evidence-based resources, current involvement (frequency and type), key enablers and barriers, and how dietitians see their future roles evolving for Net Zero.
Findings
The dissertation collected the questionnaire responses of 9 registered dietitians and found the following results:
How was Dietitians Net Zero Knowledge?
55.6% of the dietitians rated their knowledge of Net Zero as poor and those who had been in practice for longer and of a higher age category reported lower knowledge. 57% of knowledge/training barriers reported were experienced by dietitians in practice for 16 years or above. 86% of knowledge/ training barriers were reported by those who were 35-54 years old.
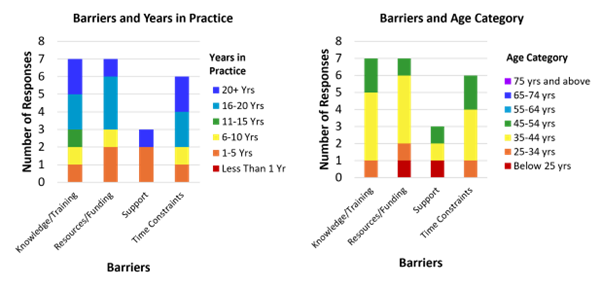
Figure 1: Stacked bar graphs showing knowledge and training barriers compared with age category and years in practice.
How Important did Dietitians feel Net Zero was?
Dietitians rated the importance of Net Zero in dietetic practice highly with 88.8% rating Net Zero as either extremely important or somewhat important. The highest ratings of importance were from dietitians working in academia or freelance.
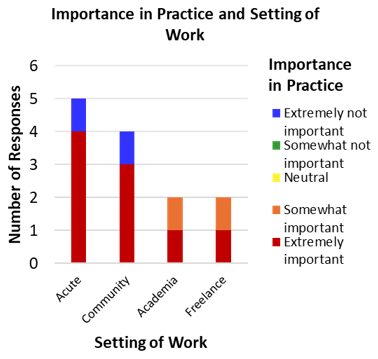
Figure 2: A stacked bar graph showing importance of Net Zero and setting of work.
Had the Dietitians Received Training on Net Zero?
Only 33.3% of the dietitians had received training on Net Zero and 66.7% had not, however those who had received training responded that it increased their involvement in Net Zero strategies, suggesting its effectiveness.
What Were Dietitians Doing to Support Net Zero?
Just over half of respondents (55.5%) reported engaging in Net Zero activities every three months or less, suggesting relatively low overall involvement. The most common actions were optimising resource use and reducing food waste, while the least frequent were contributing to policy, participating in research, and implementing low-carbon models of care.
From the qualitative responses, multiple dietitians reported advocating for Net Zero. This advocacy took various forms, such as highlighting sustainable approaches when giving dietary advice or shaping nutrition policies, promoting seasonal produce, encouraging bulk cooking, and supporting plant-based eating where appropriate.
Another common theme was resource optimisation. Examples included reducing paper use by switching to email, cutting driving-related emissions, and ensuring oral nutritional supplements (ONS) were prescribed only when necessary.
66% of gastroenterology dietitians were involved monthly or more which may have been due to a crossover of advice between gastroenterology and plant-based diets.8,15 However, advice does not always crossover, for example, for IBS.13,17 The renal specialism reported a lower involvement which was unexpected considering the benefits of a plant-based diet in renal patients and recommendations in renal guidelines. We must remember that this is a very small cohort of 9 RDs and further investigation is needed.3,10,11,14,18
Dietitians working in academic settings reported the highest levels of involvement across all types of Net Zero activity. This may be because universities play a central role in delivering the UN Sustainable Development Goals (SDGs), including SDG 12: Responsible Consumption and Production, and SDG 13: Climate Action.4,6,16 The higher engagement seen in academia may therefore reflect the forward-thinking culture of universities and their strong focus on climate action and the SDGs.5 Sustainability has been a recent addition to the dietetic curriculum.
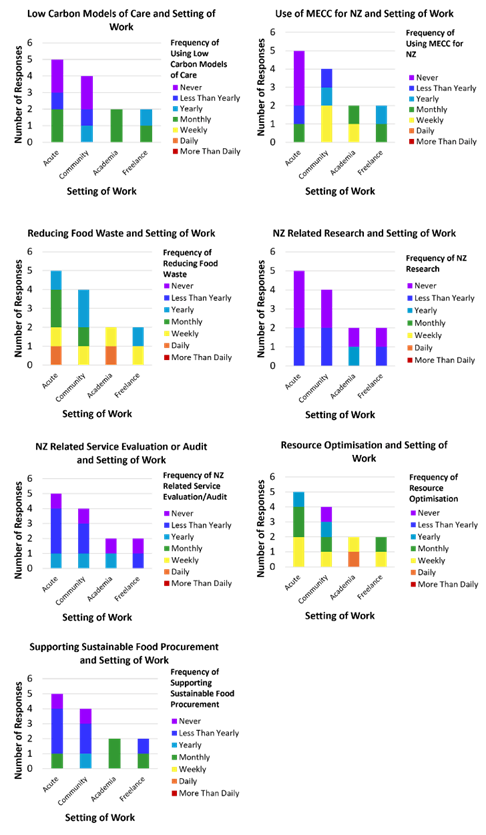
Figure 3: Stacked bar graphs showing high involvement from academic dietitians across all Net Zero activities.
What Barriers did the Dietitians Encounter?
77.8% of dietitians experienced a lack of knowledge/ training and resources (physical and educational), 66.7% experienced time constraints and 33.3% experienced a lack of support. Other barriers reported in the qualitative data were a lack of awareness and engagement in patients and dietetic colleagues, lack of support from the higher/wider healthcare system and a lack of control over unsustainable decisions.
How did the Dietitians Rate the Adequacy of Available Evidence-Based Resources?
55.5% rated the availability as poor or very poor and the mode rating was poor. A lack of educational resources was highlighted as a theme in the qualitative questionnaire responses.
How did Dietitians Think Their Roles in Net Zero Would Change in the Future?
The possibility of increased future integration of Net Zero into everyday practice was frequently suggested by participants. For example, a participant suggested ‘as we start to redo factsheets and resources, Net Zero is something we should consider.’ Others suggested more integration through ‘greater emphasis of sustainable healthcre in (university) curriculum delivery’, ‘including Net Zero in every consultation’ and ‘more plant-based diet advice’. Conversely, another participant felt that ‘with current demand on the NHS, to provide dietary advice to drive forward the Net Zero Agenda, would be difficult’.
Main Limitations of the Findings:
● The questionnaire was not piloted due to participant constraints.
● It used a small sample size of 9 dietitians.
● A convenience sampling design was used.
● The questionnaire relied on participants being truthful about being a registered dietitian.
Conclusions
● Results suggested that dietitians’ involvement was generally low but Net Zero was perceived with high levels of importance in practice.
● Dietitians mostly had poor overall knowledge and most dietitians had not received training, although the training which had been received was effective.
● The most frequent Net Zero related activities undertaken by dietitians were resource optimisation and reducing food waste and dietitians from academia showed the highest involvement of all the dietetic settings of work across all Net Zero activities.
● The most significant barriers to involvement in Net Zero is lack of knowledge/ training/resources and availability of evidence-based resources is poor.
● There are mixed opinions on the feasibility of further future integration of Net Zero into dietetic practice. While there is a directive at senior level within the NHS/healthcare to embed sustainability into practice there may be gaps in not only the education but support required by staff to deliver.
What Does this Suggest for Dietetic Practice?
This dissertation has identified that further integrating Net Zero from the start of dietetic training and implementing Net Zero training more widely and especially in dietitians with more years in practice, may increase the involvement of the profession. Using strategies such as protected time for dietitians to implement Net Zero and patient friendly Net Zero interventions could be useful to embed this into practice. Additionally, more support is needed from a department level to make it feasible to implement Net Zero.
To read the full dissertation report please click here
References:
1. British Medical Association. More support needed to help the NHS reach Net Zero. Published 2024. Accessed May 12, 2025. https://www.bma.org.uk/what-we-do/population-health/protecting-people-from-threats-to-health/more-support-needed-to-help-the-nhs-reach-net-zero#:~:text=The%20health%20service%20contributes%20around,of%20the%20public%20sector’s%20emissions
2. Copernicus. The 2024 Annual Climate Summary Global Climate Highlights 2024. Published 2025. Accessed May 18, 2025. https://climate.copernicus.eu/global-climate-highlights-2024
3. Desloovere A, Polderman N, Renken-Terhaerdt J, et al. The management of dietary fiber intake in children with chronic kidney disease – Clinical practice recommendations from the Paediatric Renal Nutrition Taskforce. J Ren Nutr. 2025;35(1):207-220. doi:10.1053/j.jrn.2024.05.008
4. Fernandes JL. Objetivos de desenvolvimento sustentável e implicações no Ensino Superior: aplicação a uma Instituição de Ensino Superior de Ciências Sociais Aplicadas. DEDiCA. 2019;15. doi:10.30827/dreh.v0i15.8032
5. Filho WL, Weissenberger S, Luetz JM, et al. Towards a greater engagement of universities in addressing climate change challenges. Sci Rep. 2023;13(1):19030. doi:10.1038/s41598-023-45866-x
6. Filho WL, Sierra J, Price E, et al. The role of universities in accelerating the sustainable development goals in Europe. Sci Rep. 2024;14(1):15464. doi:10.1038/s41598-024-65820-9
7. Health and Care Act 2022, c. 31. https://www.legislation.gov.uk/ukpga/2022/31/contents/enacted
8. Intergovernmental Panel on Climate Change. AR6 Synthesis Report Climate Change 2023. Published 2023. Accessed May 27, 2025. https://www.ipcc.ch/report/ar6/syr/downloads/report/IPCC_AR6_SYR_FullVolume.pdf
9. Mazzocchi S, Visaggi P, Baroni L. Plant-based diets in gastrointestinal diseases: Which evidence? Best Pract Res Clin Gastroenterol. 2023;62-63:101829. doi:10.1016/j.bpg.2023.101829
10. National Food Strategy. National Food Strategy: The Evidence. Published 2021. Accessed May 12, 2025. https://www.nationalfoodstrategy.org/wp-content/uploads/2021/08/NFS_Evidence-Pack.pdf
11. Navaneethan SD, Bansal N, Cavanaugh KL, et al. KDOQI US commentary on the KDIGO 2024 clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2025;85(2):135-176. doi:10.1053/j.ajkd.2024.08.003
12. Nhan J, Sgambat K, Moudgil A. Plant-based diets: a fad or the future of medical nutrition therapy for children with chronic kidney disease? Pediatr Nephrol. 2023;38(11):3597-3609. doi:10.1007/s00467-023-05875-4
13. National Health Service. Delivering a Net Zero National Health Service. NHS England; 2022. Accessed August 19, 2025. https://www.england.nhs.uk/greenernhs/a-net-zero-nhs/
14. NHS England. The NHS long term plan. Published 2019. Accessed October 25, 2024. www.longtermplan.nhs.uk/publication/nhs-long-term-plan
15. National Institute for Health and Care Excellence (NICE). Irritable bowel syndrome in adults: diagnosis and management (CG61). Published 2008. Accessed June 17, 2025. https://www.nice.org.uk/guidance/cg61/chapter/Recommendations
16. Shaw V, Anderson C, Desloovere A, et al. Nutritional management of the child with chronic kidney disease and on dialysis. Pediatr Nephrol. 2025;40(1):69-84. doi:10.1007/s00467-024-06444-z
17. SRK, Kok CW, Kunasegaran T, Ramadas A. Effect of plant-based diets on gut microbiota: a systematic review of interventional studies. Nutrients. 2023;15(6):1510. doi:10.3390/nu15061510
18. United Nations. Transforming our world: the 2030 agenda for sustainable development. Published 2015. Accessed June 14, 2025. https://docs.un.org/en/A/RES/70/1
19. DH, Paine PA, Black CJ, et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut. 2021;70(7):1214-1240. doi:10.1136/gutjnl-2021-324598
20. Wathanavasin W, Kittiskulnam P, Johansen KL. Plant-based diets in patients with chronic kidney disease. Asian Biomed (Res Rev News). 2024;18(1):2-10. doi:10.2478/abm-2024-0002
21. World Health Organization. COP26 special report on climate change and health: the health argument for climate action. Published 2021. Accessed October 25, 2024. https://iris.who.int/bitstream/handle/10665/346168/9789240036727-eng.pdf?sequence=1. Accessed October 25, 2024. https://iris.who.int/bitstream/handle/10665/346168/9789240036727-eng.pdf?sequence=1







While 88% of dietitians think Net Zero is extremely important, it seems our colleagues are mostly busy optimising paper use and suggesting seasonal produce – crucial work, but perhaps not quite the carbon-cutting revolution some might hope for! The lack of training and resources is no joke, though; its like asking us to run a marathon without proper shoes. Academia seems to be leading the charge, which makes sense – they’re probably already recycling their coffee cups. The future looks bright, but only if we get serious about training and support, otherwise, we risk being the Net Zero whisperers rather than warriors!quay random