Following on from our e-symposium, ‘Yakult Science Study Day‘, we’ve pulled together some of the key resources and references discussed within the webinar. If you missed the live webinar, you can register to watch the recording.
Yakult Science for Health

Yakult’s Scientific and Educational Site
Microbiome Matters: A podcast for healthcare professionals (HCP) to help understand more about the important community of microbes living inside us.
Diet diversity: This practical guide aims to educate HCPs about the importance of a diverse diet to promote a more diverse gut microbiota.
Skill series – Human studies: Further your understanding of key study designs used for medical and food studies in humans, and how the quality of these studies can be assessed.
Skill series – Model systems: Understand and recognise the complexities and advantages/disadvantages of different research methods including in silico computer modelling, in vitro lab studies and in vivo human studies.
Gut glossary: A dictionary for all gut-related key terms surrounding the microbiome, microbiology research and regulatory bodies, as well as key terms used throughout Study Day.
Chair: Dr Emily Prpa, Science Management, Yakult UK & Ireland

BDA GASTROENTEROLOGY SPECIALIST GROUP
BDA Food Fact Sheets: Irritable Bowel Syndrome and Diet (2022)
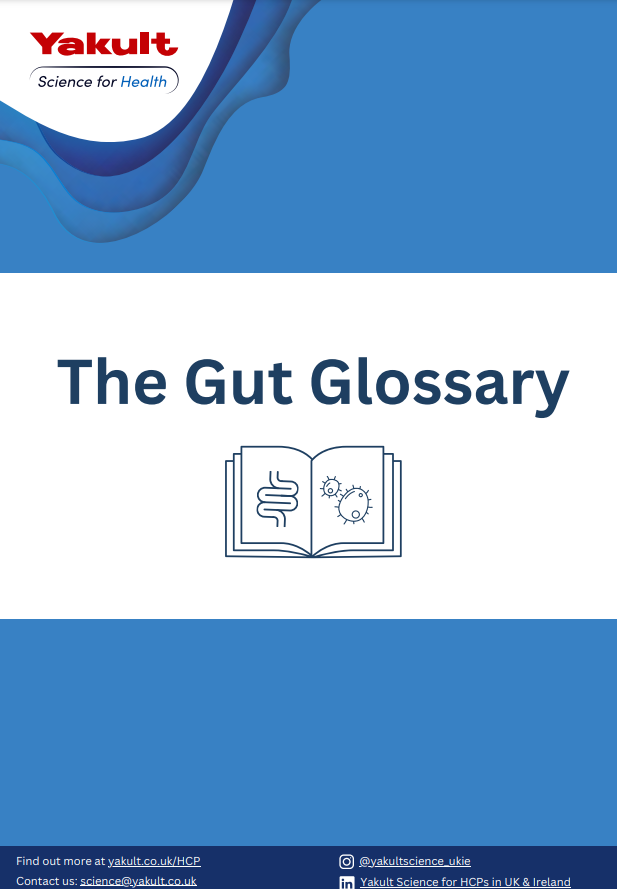
Current perspectives on gut health research: focus on prebiotics
Speaker: Professor Glenn Gibson

Guidelines:
International Scientific Association for Probiotics and Prebiotics (ISAPP)/ World Gastroenterology Organisation (WGO). Practice Guideline. Probiotics and Prebiotics (2023). Available from: https://isappscience.org/new-global-guidelines-for-probiotics-and-prebiotics-for-gut-health-and-disease/ (Accessed 01.11.2023)
Key Studies:
Arslanoglu S, Moro GE, Schmitt J, Tandoi L, Rizzardi S, Boehm G. Early dietary intervention with a mixture of prebiotic oligosaccharides reduces the incidence of allergic manifestations and infections during the first two years of life. J Nutr. 2008;138(6):1091-1095. doi:10.1093/jn/138.6.1091
Gibson GR, Hutkins R, Sanders ME, et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. 2017;14(8):491-502. doi:10.1038/nrgastro.2017.75
Other Resources:
ISSAP. 2019. Prebiotics Infographic. Available from: https://isappscience.org/wp-content/uploads/2019/04/Prebiotics_Infographic_rev1029.pdf (Accessed 30/10/202)3.
Gut microbiota and personalised nutrition: A focus on fermented foods
Speaker: Professor Paul Cotter

Key Studies:
Bourrie BCT, Ju T, Fouhse JM, et al. Kefir microbial composition is a deciding factor in the physiological impact of kefir in a mouse model of obesity. Br J Nutr. 2021;125(2):129-138. doi:10.1017/S0007114520002743
Bourrie et al. Traditional kefir reduces weight gain and improves plasma and liver lipid profiles more successfully than a commercial equivalent in a mouse model of obesity. Appl Physiol Nutr Metb. 2023 45:668. doi: 10.1016/j.jff.2018.04.039
Bourrie BC, Willing BP, Cotter PD. The Microbiota and Health Promoting Characteristics of the Fermented Beverage Kefir. Front Microbiol. 2016;7:647. Published 2016 May 4. doi:10.3389/fmicb.2016.00647
Leech J, Cabrera-Rubio R, Walsh AM, et al. Fermented-Food Metagenomics Reveals Substrate-Associated Differences in Taxonomy and Health-Associated and Antibiotic Resistance Determinants. mSystems. 2020;5(6):e00522-20. Published 2020 Nov 10. doi:10.1128/mSystems.00522-20
Lordan C, Thapa D, Ross RP, Cotter PD. Potential for enriching next-generation health-promoting gut bacteria through prebiotics and other dietary components. Gut Microbes. 2020;11(1):1-20. doi:10.1080/19490976.2019.1613124
Marco ML, Sanders ME, Gänzle M, et al. The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on fermented foods. Nat Rev Gastroenterol Hepatol. 2021;18(3):196-208. doi:10.1038/s41575-020-00390-5
Marco ML, Heeney D, Binda S, et al. Health benefits of fermented foods: microbiota and beyond. Curr Opin Biotechnol. 2017;44:94-102. doi:10.1016/j.copbio.2016.11.010
Sender R, et al. Cell. 2016;164(3):337-340; Walker and Hoyles. Nat Microbiol. 2023 Aug;8(8):1392–1396.
Walsh AM, Leech J, Huttenhower C, et al. Integrated molecular approaches for fermented food microbiome research. FEMS Microbiol Rev. 2023;47(2):fuad001. doi:10.1093/femsre/fuad001
Probiotics and the gut microbiota: key players in health?
Speaker: Professor Bruno Pot
Key Studies:
Agamennone V, Krul CAM, Rijkers G, Kort R. A practical guide for probiotics applied to the case of antibiotic-associated diarrhea in The Netherlands. BMC Gastroenterol. 2018;18(1):103. Published 2018 Aug 6. doi:10.1186/s12876-018-0831-x
Gibson GR, Hutkins R, Sanders ME, et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. 2017;14(8):491-502. doi:10.1038/nrgastro.2017.75
Hill C, Guarner F, Reid G, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506-514. doi:10.1038/nrgastro.2014.66
Oliver Chen, Marc Heyndrickx, Alexandra Meynier, Arthur Ouwehand, Bruno Pot, Bernd Stahl, Stephan Theis, Elaine Vaughan, & Michela Miani. (2023). Dietary probiotics, prebiotics and the gut microbiota in human health. Zenodo. https://doi.org/10.5281/zenodo.7590106
Salminen S, Collado MC, Endo A, et al. The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics [published correction appears in Nat Rev Gastroenterol Hepatol. 2021 Jun 15;:] [published correction appears in Nat Rev Gastroenterol Hepatol. 2022 Aug;19(8):551]. Nat Rev Gastroenterol Hepatol. 2021;18(9):649-667. doi:10.1038/s41575-021-00440-6
Sánchez B, Delgado S, Blanco-Míguez A, Lourenço A, Gueimonde M, Margolles A. Probiotics, gut microbiota, and their influence on host health and disease. Mol Nutr Food Res. 2017;61(1):10.1002/mnfr.201600240. doi:10.1002/mnfr.201600240
Swanson KS, Gibson GR, Hutkins R, et al. The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of synbiotics. Nat Rev Gastroenterol Hepatol. 2020;17(11):687-701. doi:10.1038/s41575-020-0344-2
Wang et al. The Human Microbiota in Health and Disease. Engineering. 2017. doi: https://doi.org/10.1016/J.ENG.2017.01.008
Gut-Brain Axis: Food, mood and your gut microbiome
Speaker: Dr Emily Leeming

Key Studies:
Agirman G, Hsiao EY. SnapShot: The microbiota-gut-brain axis. Cell. 2021;184(9):2524-2524.e1. doi:10.1016/j.cell.2021.03.022
Cannavale CN, Mysonhimer AR, Bailey MA, Cohen NJ, Holscher HD, Khan NA. Consumption of a fermented dairy beverage improves hippocampal-dependent relational memory in a randomized, controlled cross-over trial. Nutr Neurosci. 2023;26(3):265-274. doi:10.1080/1028415X.2022.2046963
Collins SM. A role for the gut microbiota in IBS. Nat Rev Gastroenterol Hepatol. 2014;11(8):497-505. doi:10.1038/nrgastro.2014.40
Fatahi S, Matin SS, Sohouli MH, et al. Association of dietary fiber and depression symptom: A systematic review and meta-analysis of observational studies. Complement Ther Med. 2021;56:102621. doi:10.1016/j.ctim.2020.102621
Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000;23(5):477-501. doi:10.1016/S0893-133X(00)00159-7
Lane MM, Lotfaliany M, Hodge AM, et al. High ultra-processed food consumption is associated with elevated psychological distress as an indicator of depression in adults from the Melbourne Collaborative Cohort Study. J Affect Disord. 2023;335:57-66. doi:10.1016/j.jad.2023.04.124
Lassale C, Batty GD, Baghdadli A, et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies [published correction appears in Mol Psychiatry. 2018 Nov 21;:] [published correction appears in Mol Psychiatry. 2021 Jul;26(7):3657]. Mol Psychiatry. 2019;24(7):965-986. doi:10.1038/s41380-018-0237-8
Margolis KG, Cryan JF, Mayer EA. The Microbiota-Gut-Brain Axis: From Motility to Mood. Gastroenterology. 2021;160(5):1486-1501. doi:10.1053/j.gastro.2020.10.066
Nikolova VL, Cleare AJ, Young AH, Stone JM. Updated Review and Meta-Analysis of Probiotics for the Treatment of Clinical Depression: Adjunctive vs. Stand-Alone Treatment. J Clin Med. 2021;10(4):647. Published 2021 Feb 8. doi:10.3390/jcm10040647
Opie RS, O’Neil A, Jacka FN, Pizzinga J, Itsiopoulos C. A modified Mediterranean dietary intervention for adults with major depression: Dietary protocol and feasibility data from the SMILES trial. Nutr Neurosci. 2018;21(7):487-501. doi:10.1080/1028415X.2017.1312841
Zamani M, Alizadeh-Tabari S, Zamani V. Systematic review with meta-analysis: the prevalence of anxiety and depression in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2019;50(2):132-143. doi:10.1111/apt.15325
Zhang Q, Chen B, Zhang J, et al. Effect of prebiotics, probiotics, synbiotics on depression: results from a meta-analysis. BMC Psychiatry. 2023;23(1):477. Published 2023 Jun 29. doi:10.1186/s12888-023-04963-x
Menopause, hormones and the gut microbiome
Speaker: Brandilyn A. Peters-Samuelson

Key Studies:
Ervin SM, Simpson JB, Gibbs ME, et al. Structural Insights into Endobiotic Reactivation by Human Gut Microbiome-Encoded Sulfatases. Biochemistry. 2020;59(40):3939-3950. doi:10.1021/acs.biochem.0c00711
Łaniewski P, Herbst-Kralovetz MM. Connecting microbiome and menopause for healthy ageing. Nat Microbiol. 2022;7(3):354-358. doi:10.1038/s41564-022-01071-6
Peters BA, Santoro N, Kaplan RC, Qi Q. Spotlight on the Gut Microbiome in Menopause: Current Insights. Int J Womens Health. 2022;14:1059-1072. Published 2022 Aug 10. doi:10.2147/IJWH.S340491
Peters BA, Lin J, Qi Q, et al. Menopause Is Associated with an Altered Gut Microbiome and Estrobolome, with Implications for Adverse Cardiometabolic Risk in the Hispanic Community Health Study/Study of Latinos. mSystems. 2022;7(3):e0027322. doi:10.1128/msystems.00273-22
Wilmanski T, Diener C, Rappaport N, et al. Gut microbiome pattern reflects healthy ageing and predicts survival in humans [published correction appears in Nat Metab. 2021 Apr;3(4):586]. Nat Metab. 2021;3(2):274-286. doi:10.1038/s42255-021-00348-0
The Gut:Skin Axis
Speaker: Natalie Yerlett

Guidelines:
International Scientific Association for Probiotics and Prebiotics (ISAPP)/ World Gastroenterology Organisation (WGO). Practice Guideline. Probiotics and Prebiotics (2023). Available at: https://isappscience.org/new-global-guidelines-for-probiotics-and-prebiotics-for-gut-health-and-disease/ (Accessed 01.11.2023)
Key Studies:
Ahn K. The Effect of Prebiotics on Atopic Dermatitis. Allergy Asthma Immunol Res. 2023;15(3):271-275. doi:10.4168/aair.2023.15.3.271
Corcione S, Lupia T, De Rosa FG; Host and Microbiota Interaction Study Group (ESGHAMI) of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID). Microbiome in the setting of burn patients: implications for infections and clinical outcomes. Burns Trauma. 2020;8:tkaa033. Published 2020 Aug 14. doi:10.1093/burnst/tkaa033
De Pessemier B, Grine L, Debaere M, Maes A, Paetzold B, Callewaert C. Gut-Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions. Microorganisms. 2021;9(2):353. Published 2021 Feb 11. doi:10.3390/microorganisms9020353
Mahmud MR, Akter S, Tamanna SK, et al. Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut Microbes. 2022;14(1):2096995. doi:10.1080/19490976.2022.2096995
Oh J, Byrd AL, Park M; NISC Comparative Sequencing Program, Kong HH, Segre JA. Temporal Stability of the Human Skin Microbiome. Cell. 2016;165(4):854-866. doi:10.1016/j.cell.2016.04.00854-66
Reimer-Taschenbrecker A, Künstner A, Hirose M, et al. Predominance of Staphylococcus Correlates with Wound Burden and Disease Activity in Dystrophic Epidermolysis Bullosa: A Prospective Case-Control Study. J Invest Dermatol. 2022;142(8):2117-2127.e8. doi:10.1016/j.jid.2022.01.020
Yerlett N, Petrof G, Bageta M, Balboa PL, Martinez AE. The impact of using a multistrain probiotic supplement on gastrointestinal function in children and adolescents with severe recessive dystrophic epidermolysis bullosa [published online ahead of print, 2022 Nov 11]. Clin Exp Dermatol. 2022;llac070. doi:10.1093/ced/llac070lesecents
Zhang M, Jiang Z, Li D, et al. Oral antibiotic treatment induces skin microbiota dysbiosis and influences wound healing. Microb Ecol. 2015;69(2):415-421. doi:10.1007/s00248-014-0504-4
Faecal microbiota transplants: how it works and why it doesn’t
Speaker: Dr James Kinross

Guidelines:
Lopetuso LR, Deleu S, Godny L, et al. The first international Rome consensus conference on gut microbiota and faecal microbiota transplantation in inflammatory bowel disease. Gut. 2023;72(9):1642-1650. doi:10.1136/gutjnl-2023-329948
Mullish BH, Quraishi MN, Segal JP, et al. The use of faecal microbiota transplant as treatment for recurrent or refractory Clostridium difficile infection and other potential indications: joint British Society of Gastroenterology (BSG) and Healthcare Infection Society (HIS) guidelines. Gut. 2018;67(11):1920-1941. doi:10.1136/gutjnl-2018-316818
Key Studies:
El-Salhy M, Hatlebakk JG, Gilja OH, Bråthen Kristoffersen A, Hausken T. Efficacy of faecal microbiota transplantation for patients with irritable bowel syndrome in a randomised, double-blind, placebo-controlled study. Gut. 2020;69(5):859-867. doi:10.1136/gutjnl-2019-319630
Davar D, Dzutsev AK, McCulloch JA, et al. Fecal microbiota transplant overcomes resistance to anti-PD-1 therapy in melanoma patients. Science. 2021;371(6529):595-602. doi:10.1126/science.abf3363
Fuentes S, Rossen NG, van der Spek MJ, et al. Microbial shifts and signatures of long-term remission in ulcerative colitis after faecal microbiota transplantation. ISME J. 2017;11(8):1877-1889. doi:10.1038/ismej.2017.44
Ianiro G, Punčochář M, Karcher N, et al. Variability of strain engraftment and predictability of microbiome composition after fecal microbiota transplantation across different diseases. Nat Med. 2022;28(9):1913-1923. doi:10.1038/s41591-022-01964-3
Imdad A, Nicholson MR, Tanner-Smith EE, et al. Fecal transplantation for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2018;11(11):CD012774. Published 2018 Nov 13. doi:10.1002/14651858.CD012774.pub2
Mullish BH, McDonald JAK, Pechlivanis A, et al. Microbial bile salt hydrolases mediate the efficacy of faecal microbiota transplant in the treatment of recurrent Clostridioides difficile infection. Gut. 2019;68(10):1791-1800. doi:10.1136/gutjnl-2018-317842
Shkoporov AN, Clooney AG, Sutton TDS, et al. The Human Gut Virome Is Highly Diverse, Stable, and Individual Specific. Cell Host Microbe. 2019;26(4):527-541.e5. doi:10.1016/j.chom.2019.09.009
Van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407-415. doi:10.1056/NEJMoa1205037
Wrønding T, Vomstein K, Bosma EF, et al. Antibiotic-free vaginal microbiota transplant with donor engraftment, dysbiosis resolution and live birth after recurrent pregnancy loss: a proof of concept case study. EClinicalMedicine. 2023;61:102070. Published 2023 Jun 26. doi:10.1016/j.eclinm.2023.102070







Specifically, are there any groundbreaking findings or emerging trends in microbiome research discussed during the event that could impact healthcare practices or dietary recommendations? Tel U
The full day is available for health professionals to watch on demand: https://mynutriweb.com/yakult-science-study-day/