 This week (9-15th May 2022) is #CoeliacAwarenessWeek and we’ve invited award winning specialist dietitian Cristian Costas Battle to explore the link between coeliac disease and type 1 diabetes. What challenges do patients have when they are diagnosed with both conditions and how can we support them? The article includes input from Coeliac UK sharing their resources to help manage both conditions and also Dietitian Chris Cheyette. Let us know in the comments if you have any great resources you use in practice and what you find helps your patients.
This week (9-15th May 2022) is #CoeliacAwarenessWeek and we’ve invited award winning specialist dietitian Cristian Costas Battle to explore the link between coeliac disease and type 1 diabetes. What challenges do patients have when they are diagnosed with both conditions and how can we support them? The article includes input from Coeliac UK sharing their resources to help manage both conditions and also Dietitian Chris Cheyette. Let us know in the comments if you have any great resources you use in practice and what you find helps your patients.
What is Coeliac Disease?
Coeliac Disease (CD) is an autoimmune condition where gluten triggers an immune reaction, causing damage to the small intestine when eaten. Currently, a gluten free diet is the only treatment available and it needs to be followed for life to keep the small intestine healthy, stay symptom free and reduce the risk of further complications. Research shows that people with coeliac disease can eat foods which contain no more than 20 parts per million of gluten. This means that gluten needs to be avoided in foods from an ingredient point of view as well as taking into consideration cooking and manufacturing methods that can cross-contaminate gluten free foods.
What is the link between Coeliac Disease and Type 1 Diabetes?
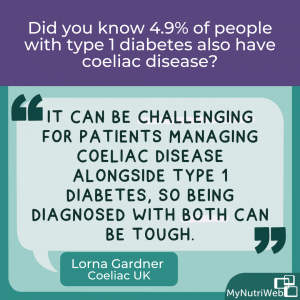
Since CD is an autoimmune condition, it is associated with some other autoimmune conditions like Type 1 Diabetes (T1DM) and thyroid disease. T1DM has been shown to be one of the autoimmune conditions that is most linked with CD. Around 4-9% of people with T1DM have CD and therefore people with T1DM should be screened for coeliac disease at diagnosis of T1DM.
Which condition tends to get diagnosed first?
Both conditions can appear at any point in life. However, most people will likely be diagnosed with T1DM before they get diagnosed with CD. T1DM is usually diagnosed in younger children and adults under the age of 40, whereas CD is most often diagnosed in age groups of 40-60. Furthermore, symptoms of CD can be digestive and non-digestive and vary in severity. Some symptoms can include fatigue, abdominal pain, diarrhoea, unexplained weight loss, mouth ulcers and headaches, though some people can also be asymptomatic. Due to challenges in testing, symptoms that are common to other conditions and other factors, it takes on average 13 years to get a diagnosis of CD.
What signs and symptoms are linked to Type 1 diabetes?
When it comes to T1DM, there can be a crossover of two symptoms that can also appear in CD, which are unexplained weight loss and excessive fatigue. Some of the other symptoms of T1DM people can experience include:
- Feeling very thirsty
- Passing a lot of urine (especially on a night)
- Having blurred vision
- Having fruity-smelling breath
- Noticing that cuts and grazes don’t heal
- Some people can also get genital itching or thrush
Is there a link between Coeliac Disease and Type 2 diabetes?
To this day, there is no evidence to suggest that having CD increases the risk of developing Type 2 diabetes, mainly because Type 2 diabetes is not an autoimmune condition. However, if people with coeliac disease make adequate diet and lifestyle choices despite being on a gluten free diet, they can reduce the risk of developing Type 2 diabetes in a similar way the general population can.
How difficult is it to live with Coeliac Disease and Type 1 Diabetes?
For someone living with both type 1 diabetes and coeliac disease there is undoubtedly a greater burden, in terms of both decision making, and day-to-day tasks. This ranges from extra time for meal planning, shopping and calculating carbohydrate intake to more hospital appointments. Management of food intake is central to both long-term conditions. For some people this can add to the psychological strain, as food becomes a key factor in day-to-day choices. People may feel excluded from eating out or enjoying special occasions.
Chris Cheyette, Registered Dietitian and Author of ‘Carbs and Cals’
I feel it is key that we have resources that help people navigate daily decision making and food planning. The Carbs & Cals resources (www.carbsandcals.com) provide carbohydrate and other nutrient information on some generic gluten free foods. We have plans to grow our app food database to include more in the future, including some common gluten free brands.
Having adequate resources and support to help manage these conditions is key. Otherwise people will feel the dietary treatment is more complicated than it needs to be and this can further increase the psychological burden for both conditions. This can make people feel like the diet therapies for both conditions cannot possibly co-exist because gluten free branded foods could potentially be driving blood glucose higher, as well as potentially being unhealthier.
Lorna Gardner, Membership Helpline Dietitian of Coeliac UK
“It can be challenging for patients managing coeliac disease alongside type 1 diabetes, so being diagnosed with both can be tough. As part of our Coeliac UK Awareness Week we are highlighting the fact that the condition affects 1 in 100 people but only 36% are diagnosed, we also know that 4-9% of people with type 1 diabetes have coeliac disease.
Our aim is to raise awareness of coeliac disease to increase the rate of diagnosis and stop this unnecessary suffering – our campaign #ShineALightOnCoeliac, spotlights the key symptoms to watch for, and when to test – at point of diagnosis for type 1 diabetes being one such time.
So, how can we help people with these two conditions move forward?
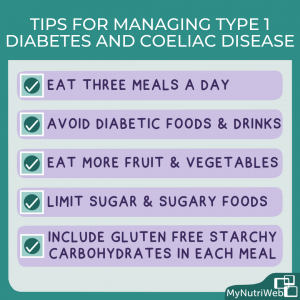
Whilst it’s important to acknowledge these challenges, it’s also important to help people understand that they don’t need to follow two different diets. By helping people focus on naturally gluten free foods, they can focus on foods like fruits, vegetables, pulses, gluten free grains, nuts, seeds, dairy, lean meats, poultry and fish as well as healthy fats- which can indeed lead to a healthy diet long-term. Focusing on naturally gluten free foods can also take some of the pressure off having to constantly read food labels in depth to check for carbohydrate content and gluten. Furthermore, using the Coeliac UK’s Food Checker app will also make it easier to identify gluten free foods outside the gluten free section in supermarkets. The use of accurate and official apps for both conditions can be a great help. However, getting to a point where these two conditions can be managed with confidence for every food interaction certainly does require substantial nutrition education.
Resources to help manage both conditions
Coeliac UK Resources:
A useful resource is Coeliac UK’s factsheet on Coeliac Disease and Type 1 Diabetes which gives ten top diet tips for managing both conditions:
LornaGardner
For Healthcare Professionals we have free CPD on coeliac disease available at https://www.coeliac.org.uk/healthcare-professionals/cpd/
In addition, we have a number of resources, including a simple summary of diagnosis and management of coeliac disease https://www.coeliac.org.uk/document-library/7037-one-page-summary–diagnosis-and-management-infographic/ and also provide useful updates in through our Healthcare Professional Network https://www.coeliac.org.uk/join-us/membership/hcp/
For patients, on our website and as part of the membership, we also have useful aids around selecting suitable foods:
Food and Drink information on over 150,000 gluten free and mainstream foods that can be included in the diet. Within our online information, you can check the nutritional information for many individual products to find out the carbohydrate content per 100g.
Home of Gluten Free Recipes: where you can filter for recipes that have a good source of fibre or are low in fat. Some of our recipes include the total carbohydrate per serving. Some recipes have free access, and additional content is made available to our members, with membership at £1.25 per month.
For those who think they may have coeliac disease we have an online self assessment tool https://isitcoeliacdisease.org.uk/
Other useful resources include:
Coeliac Disease and Diabetes. Diabetes UK – A guide from UK charity specific for managing both conditions
Living with Coeliac and Diabetes Guide. Glutafin. 15 page booklet giving advice for individuals living with both conditions
Diabetes UK Recipe Finder – Recipes suitable for diabetes showing the carbohydrate amounts per serving, with over 100 gluten-free recipes. Examples include:
- Rice and Beans
- Roasted Cauliflower, paneer and chickpea curry
- Warm Lentil and Goat’s Cheese Salad
- Tomato, olive, asparagus and bean salad
- Spicy Potato Wedges
- Saag Aloo
- Roasted Peppers with Feta Cheese
- Parmesan Parsnips
Carbs and Cals (2016) – Chris Cheyette. Expert-approved visual guide showing at-glance calorie and nutrient contents for hundreds of foods and drinks
Living with Coeliac Disease and Diabetes. Glutafin. This is a really useful leaflet for patients about managing both conditions and also provides some gluten free recipes with nutritional information available
Gluten Free Food Checker App. Coeliac UK’s award winning app to allow for easy identification of suitable foods for a gluten free diet
How should dietitians and other health professionals be involved?
We must never forget that food plays a key role in people’s quality of life. Therefore, we should always try to find ways of making diets as inclusive as possible despite the dietary restrictions needed. This includes finding ways to help people enjoy eating out and finding ways to help people have foods in their diet that they enjoy whilst also being able to have meals with friends and family. There is so much more to these diet therapies than simply carbohydrate counting or avoiding gluten. It’s about making these diets as safe, inclusive and balanced as possible.
Therefore, we have to acknowledge that our individual knowledge and experience alone may not be enough to support these patients as best as possible. We may need to work with other health professionals who can share more knowledge, tools and resources to make diet therapy easier for the patient. This is where it can be helpful to refer to specialist dietitians for each condition, consider support groups for peer support and also be open to collaborative working across different specialities to get the best outcome for the patient, depending on each patient’s needs.
In conclusion, prompt screening and adequate support are crucial for these two conditions. We must never underestimate the psychological burden of having to restrict diet in two different ways for life for those living with coeliac disease and Type 1 Diabetes. This is why we always have to be open to collaborative working across different specialities to get the best outcome for the patient.
Related MyNutriWeb Content
Understanding Coeliac Series (2022) – Part 1 (Diagnosis and Management) and Part 2 (Deep Dive into the Gluten Free Diet) . Supporting Resources Blog.
Coeliac Disease – Tips for a Sustainable Gluten Free Diet (2022) – Blog post by Cristian Costas Battle into whether sustainable eating is possible when avoiding gluten






