
Adele Hug, Registered Dietitian, sorts the facts through the minefield of misinformation around cancer and nutrition
As a cancer dietitian, there is rarely a day that goes by when I’m not asked if ‘sugar feeds cancer’? Too often, this is answered with a ‘No, don’t worry about that” when the actual answer is far more complex and why people are desperate to know is not that simple either.
Macmillan estimate one in two of us will be diagnosed with cancer during our lifetime but a cancer diagnosis is still unexpected, feared and confusing. Let’s dive deep to uncover if there is any truth in some of the most common myths around nutrition and cancer – and why they exist at all.
It’s also important to explore complementary and alternative therapies/medicines (CAMs), and the difference between them.
Why are there so many myths about nutrition and cancer?
We know nutrition is rife with pseudoscience – and cancer is no exception.
Nutrition is often one of the only factors a person can control when undergoing numerous scans, surgeries and treatments (or watching their loved one go through these). So understandably, people are seeking information, support and hope. Often their (Google!) search leads them to ‘cancer cures’ or ‘immune boosting supplements’, and someone either trying to help with a tip that helped their neighbour’s sister, or worse, making money touting ‘cures that Big Pharma didn’t want you to know about’.
Conventional cancer treatments include those with a strong evidence base with well-designed clinical trials within certain tumour types, such as chemotherapy, radiotherapy, targeted therapies, immunotherapies and stem cell transplants.
But it’s estimated that 48–88% of people with cancer use complementary and alternative therapies/medicine (CAMs). Whilst the lines blur between the two, the table below provides some definitions and differences. See Cancer Research UK for more detail.
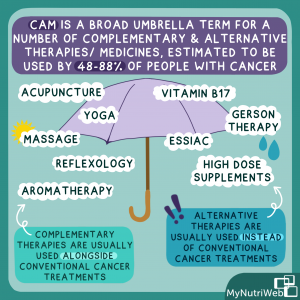
| CAM | Examples | Benefits | Risks |
| Complementary therapies (CT)
Used alongside conventional cancer treatments
|
Acupuncture
Aromatherapy Massage Reflexology |
Improved feeling of autonomy and hope
Improve symptoms/side effects Support nutritional status and physical fitness Enhance psychological health and coping
|
Evidence base is still growing
Small number of practitioners promoting alternative therapies practice in the CT space. |
| Alternative therapies (AT)
Used instead of conventional cancer treatments |
Vitamin B17
High dose supplements like Vitamin C
Plus any CT that is used instead of convention cancer treatments |
Improved feeling of autonomy and hope
|
Increased risk of malnutrition
Known and unknown interactions with treatment May be expensive
|
Do I need to worry about CAM as a nutrition professional?
It depends! Just like cancer refers to over 200 different diseases, CAM is a very broad umbrella term – we need to support people living with cancer and carry out a risk assessment on each individual case to provide person-centred care.
How do you support someone investigating or following a CAM diet?
Many do not disclose they might be using CAM to their health professional. It’s a privilege if you are working with someone who has trusted you enough to tell you. Listening to them, understand their why and assess any risks to what they are following to start an open conversation. You can talk about:
- Your role and how you work within an evidence base and explain your scope of practice we deliver as registered professionals
- Be honest – we don’t know it all! Nutrition evidence is and will continue to constantly change and as long as there isn’t too great a risk in what someone is following, be there for them!
- Work with them to meet safe goals that meet their nutritional needs
- Don’t be afraid to admit you don’t know and refer on or seek clinical supervision
So what are some of the common cancer nutrition myths and is there any truth to them?
1: Does sugar ‘feed’ cancer? And if so, does cutting sugar out of the diet, or following a ketogenic diet, ‘starve’ the cancer?
Firstly, where did this idea come from? Warburg who won a Nobel Prize back in 1931 for his research that showed tumours can metabolise glucose anaerobically, rather than aerobically, even when O2 is available – it’s known as the Warburg Effect. And you only need to look at a PET scan to literally see tumour/s metabolising glucose. No wonder people ask if sugar feeds cancer.
What are the facts?
Tumours are complex and the pathways for nutrition are too – cutting out one food group doesn’t ‘starve’ the cancer cells – in fact, this risks nutrient deficiencies and malnutrition that can really impact treatment outcomes and quality of life.
In reality, tumours use ALL the nutrients that ‘normal’ cells do – carbohydrates, protein, fats, vitamins, minerals and more. There is an entire treatment type that stops the tumours ability to get this nutrition, by stopping its ability to grow new blood vessels – a process known as angiogenesis.
What about keto – is there evidence?
A systematic review in 2017 summarised what we know – but evidence is very sparce and often only based on research on rodents. There are some small pilot studies emerging (Elles et al& Schwartz et al) investigating the feasibility and safety of adjuvant ketogenetic diets in brain cancer (alongside standard ‘conventional’ treatment). Unsurprisingly to many of us, compliance was an issue, and these are well supported patients on a trial, rather than free living people with cancer, but they were safe alongside conventional treatment. Watch this space – I am, as I suspect ongoing larger trials in this space.
My top tip
For most people with and beyond cancer, eating more plants is a good way to go – this includes a variety of carbohydrate and fibre-rich foods. Carbs – yes including sugar – are an important energy source to allow recovery from treatment and enable people to move their bodies more and do the things they love!
2. Is an alkaline diet the way to eat to cure cancer? NO…but.. let’s take a look!
Where did this idea come from?
This comes from the idea that foods have an acidic (meat/fish/eggs/alcohol), neutral (‘natural’ fats, starch, sugar) or alkaline (fruits, nuts, vegetables, pulses) ‘leftover’ when metabolised, and cancer cells thrive in an acidic environment – therefore eating more alkaline foods results in an environment that the tumour would not survive in.
What are the facts?
There are almost no studies into alkaline diets and cancer! But parts of the diet such as including more plant-based foods, having moderate fats and less booze can be low risk additions to the diet (and a positive change for many people)! However, the idea to rely on a strict diet to control internal pH is very risky, humans are equipped with organs that keep our pH in tight control – let’s rely on those.
What are the concerns?
When followed to the extreme (which can involve inaccurate urine dipsticks), there is a risk of severe dietary restrictions. There are even some clinics that offer IV bicarbonate soda to increase the alkalinity of the body – this is super risky and has resulted in death – and not enough jail time for the ‘doctor’ who delivered it.
3. Does dairy cause cancer? NO, in fact it may be protective – but research is ongoing!
Dairy and cancer have quite the history. Dairy has been and continues to be questioned on its role in cancer prevention and progression, especially for people with breast cancer.
Where did this idea come from?
The idea is that hormones in the production of, and present in, dairy foods promote hormone receptor positive cancers. There was a big appetite for dairy-free diets in the 1990s and 2000s. First there was Professor Jane Plant’s anecdotal no dairy regime for her own breast cancer. Then the now widely debunked China Study continued to link dairy to cancers in the ‘Western world’.
What is the evidence and how it should be applied?
It is often a surprise that systematic reviews of the evidence suggest that dairy may be protective against premenopausal breast and bowel cancers. Cohort observation studies continue (Fraser et al and Nakansiki et al) have conflicting results but dairy is considered safe by WCRF and research is ongoing into dairy as a whole, individual dairy foods (such as milk vs yoghurt) and foods containing calcium.
My top tip
For many, dairy may not be something they want to or feel comfortable to include in their diets, for many reasons – explore this. Our job is to make sure they have enough:
- Calcium
- Vitamin D
- Protein
- Fluid
4. Does soya cause cancer? NO…It’s another common myth that soya foods cause cancer.
Where did this idea come from?
This has come from the knowledge that soya beans contain isoflavones, a phytoestrogen. Phytoestrogens have a similar chemical structure to the human hormone oestrogen. This led to concerns that soya foods may be a ‘promoter’ for oestrogen receptor positive cancers (ER+ breast cancers).
What are the facts?
It is now understood that within the human body, isoflavones do not behave the same way as oestrogen. In fact, recent comprehensive reviews into breast cancer survival by the World Cancer Research Fund (WCRF) conclude that soya foods are safe, and may improve survival after a primary breast cancer diagnosis. There is a growing body of evidence on not only the safety of soya, but its many nutritional benefits.
My top tip
Soya foods are plant-based and can be a great first step for someone exploring more plant-based eating alongside a cancer diagnosis, especially as, for example, soya milk has a comparable amount of protein to dairy milk. But as with dairy, some people may not want to eat soya foods, so ensuring their diet is nutritionally complete is what is important.
So what do we know about food and cancer?
Well, it’s complex! The evidence is moving towards diet variety and quality, more plants (but not exclusively) and higher protein needs alongside treatments. Plus, we need to step away from individual nutrients and look more into the wider determinants of health.
While there are lots of exciting studies on the horizon into CAMs, we are a long way away from adding these into standard treatments.
And with many people unaware of the links between alcohol and cancer risk there’s much more work to be done to support systemic change for the risks we know more about, while continuing to research things that we need to understand more.
What do I see in the future for the field of nutrition and cancer?
I think we need to understand more about the individual makeup of a tumour, its genetic components, surface protein receptors and the tumour microenvironment. Then we MIGHT be able to start to understand the impact of different dietary components (such as amino acids) on tumour growth to create more personalised nutritional plans.
However, this is currently a pipe dream. What we do know is that food is important to fuel and support our body and its functions. A healthy balanced diet can help the body to cope with and recover well from researched treatments that have the best chance of controlling cancer, with improved overall survival and quality of life.
My top tips for navigating around nutrition and cancer:
- How risky is the diet being followed?
- Be critical of the evidence and the general advice – know where guidelines are using an assumption
- Be honest about the gaps within the evidence base
- Be ready for the future
Helpful links and further reading:
- Trekstock – Food & Cancer: What’s the Deal?
- Life Kitchen – https://lifekitchen.co.uk
- Search individual supplements/herbs on Memorial Sloan Kettering Cancer Centre
- Cancer Research UK (2022) – Complementary and Alternative Therapies
- ESPEN Practical (2021) ESPEN Practical Guidelines in Cancer Nutritional Care
- BDA Oncology (2021) – Challenging Cancer Myths
- MyNutriWeb (2021) – Guidance on Soya
- WRCF (2018) – Cancer Update Programme
Related MyNutriWeb content
Plant-based diet and bowel cancer (2022) – Blog post
Bowel cancer and red meat (2021) – 60 mins webinar and Key Resources
Alcohol and Cancer (2021)- 60 mins webinar and Key Resources
Breast Cancer and Diet (2021)- 60 mins webinar
Eating well after Cancer (2021) – 60 mins webinar and Key Resources
Breast cancer: Using diet and lifestyle to reduce risk and recurrence (2021) – Blog post







What a comprehensive and useful article. I particularly like the inclusion of where the myth could have originated. Thank you!
Useful information. Debunking some myth and reminding that the entire diet is important and not individual food,
Super article – concise and comprehensive