 By Abi Lester, Senior Events and Project Manager at Pancreatic Cancer UK & Dianne Dobson, Pancreatic Cancer Specialist Nurse, Pancreatic Cancer UK
By Abi Lester, Senior Events and Project Manager at Pancreatic Cancer UK & Dianne Dobson, Pancreatic Cancer Specialist Nurse, Pancreatic Cancer UK
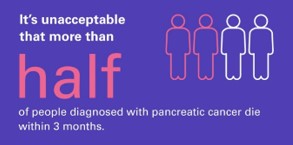
Did you know, more than half of people diagnosed with pancreatic cancer die within 3 months? November is Pancreatic Cancer Awareness Month and this blog aims to equip health professionals with information and resources to help when managing individuals with pancreatic cancer.
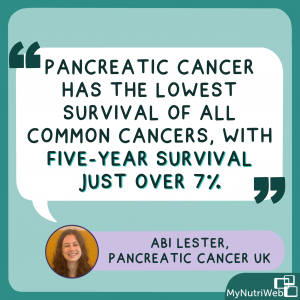
Pancreatic cancer is the 10th most common cancer with over 10,000 people diagnosed every year in the UK.
It is the 5th biggest cancer killer with 9,000 deaths every year and is predicted to become the 4th biggest cancer killer by 2026.
Pancreatic cancer has the lowest survival of all common cancers, with five-year survival just over 7%.
- 1 in 4 people diagnosed with pancreatic cancer will die within one month
- 1 in 2 people diagnosed die within 3 months
- 3 in 4 people will die within a year `
There has been no significant change in overall survival for over 50 years.
The nutritional issues patients may experience
Pancreatic cancer causes disruption to both the exocrine and endocrine function of the pancreas. This affects the production of digestion hormones (exocrine) and disruption of insulin/glucose metabolism (endocrine) in the majority of people affected by this disease.
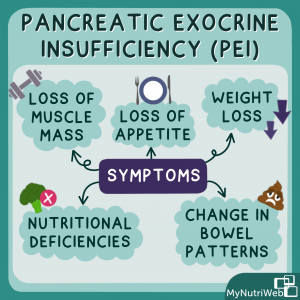
Pancreatic cancer can cause pancreatic exocrine insufficiency (PEI). This occurs when the pancreas is unable to produce sufficient enzymes or produce them at the right time to ensure adequate digestion. If the pancreas is unable to produce and release digestive enzymes the nutrients in food will not be digested. This can lead to gastrointestinal symptoms including:
- Loss of appetite
- Weight loss
- Loss of muscle mass
- Nutritional deficiencies
- Change in bowel patterns
These debilitating symptoms are often present at diagnosis, impacting patient outcomes including quality of life and overall survival in addition to the ability to undertake treatment.
PEI occurs in up to 90% of people with pancreatic cancer, even if patients do not have it at the time of diagnosis, most will develop it during the course of their disease. Early treatment of PEI is recommended to reduce symptoms and improve fat absorption and weight gain in patients with pancreatic cancer. The main treatment for PEI in pancreatic cancer is pancreatic enzyme replacement therapy (PERT).
Pancreatic enzyme replacement therapy (PERT)
PERT is available in capsules that replace the enzymes that the pancreas would normally make. PERT formulations contain lipase (digest fats), amylase (digest carbohydrates) and protease (digest proteins). These help people with pancreatic cancer to digest their food by breaking down carbohydrates, fats and proteins in food.
PERT mimics the normal physiology of pancreatic enzyme action.
It can help manage the symptoms of problems with digestion, such as weight loss or diarrhoea. It can also help patients to cope better with treatments, such as chemotherapy or surgery.
By managing these problems with diet and digestion, it can make a big difference to how people feel and their quality of life.
Type 3C Diabetes
The disruption in glucose/insulin production in patients with pancreatic cancer will often result in a diagnosis of type 3c Diabetes (or pancreatogenic diabetes).
In comparison with Type 1 or Type 2 diabetes, Type 3c diabetes results in lack of both insulin and glucagon production. These patients will often present with a change in glycaemic control (if known diabetic) at the time of diagnosis, and may be frequently referred to as ‘brittle diabetics’.
There is a lot of information about losing weight for people with type 2 diabetes – this won’t be relevant to people with type 3c diabetes who have lost weight or are struggling to put weight back on.
Those people with a diagnosis of Type 3c diabetes require expert dietitian and diabetic management to ensure adequate glycaemic management in addition to PERT management. Use of steroids during treatment (ie chemotherapy regimens) will also impact on management of diabetes throughout the course of treatment.
Resources
Resources for you
External resources
- For more detailed information on testing for and diagnosing PEI, read the Consensus for the management of pancreatic exocrine insufficiency: UK practical guidelines.
- What is Type 3C diabetes – https://www.diabetes.org.uk/diabetes-the-basics/type-3c-diabetes
- Type 3C diabetes and healthy living – https://www.pancreaticcancer.org.uk/wp-content/uploads/2020/10/Type-3c-diabetes-and-healthy-living.pdf
Pancreatic Cancer UK courses
- To learn more about pancreatic cancer you can take our free 3-part Introduction to Pancreatic Cancer course for health professionals
- Or have a look at our free health professionals guide to PERT
Resources for your patients
Pancreatic Cancer UK sessions and webinars
- Our online support sessions give patients a chance to talk to others with pancreatic cancer and one of our specialist nurses about a specific area, we run one of these on managing nutrition and pancreatic enzymes
- We also run webinars for patients on different topics and always record so people can watch in future, feel free to share our ‘pancreatic cancer and diabetes’ and our ‘ask a dietitian’ webinar
Pancreatic Cancer UK information
RELATED MYNUTRIWEB CONTENT
Diet and Cancer Myths (2022). Blog post exploring myths
Enjoying Food With Cancer (2022) – MyNutriKitchen with Life Kitchen and Adele Hug
Plant-based diet and bowel cancer (2022) – Blog post
Bowel cancer and red meat (2021) – 60 mins webinar and Key Resources
Alcohol and Cancer (2021)- 60 mins webinar and Key Resources
Breast Cancer and Diet (2021)- 60 mins webinar
Eating well after Cancer (2021) – 60 mins webinar and Key Resources
Breast cancer: Using diet and lifestyle to reduce risk and recurrence (2021) – Blog post







nice article, mind sharing inbox.
Regards.
very insightful